You just finished a big meal and you lie down on the couch for some much needed rest. All is well for a short period of time and then suddenly the pain begins. Starting at your breastbone and moving toward your throat is a burning ache. You have heartburn again. This is happening more and more often and you are unsure what to do. You hate to miss time from work to go to the doctor for a little indigestion. However, this discomfort can be a sign of something bigger – Gastroesophageal Reflux Disease or GERD. GERD can have consequences beyond simple heartburn, including difficulty with asthma-like symptoms, chronic cough, voice disorders, injury to the esophagus and difficulty swallowing.
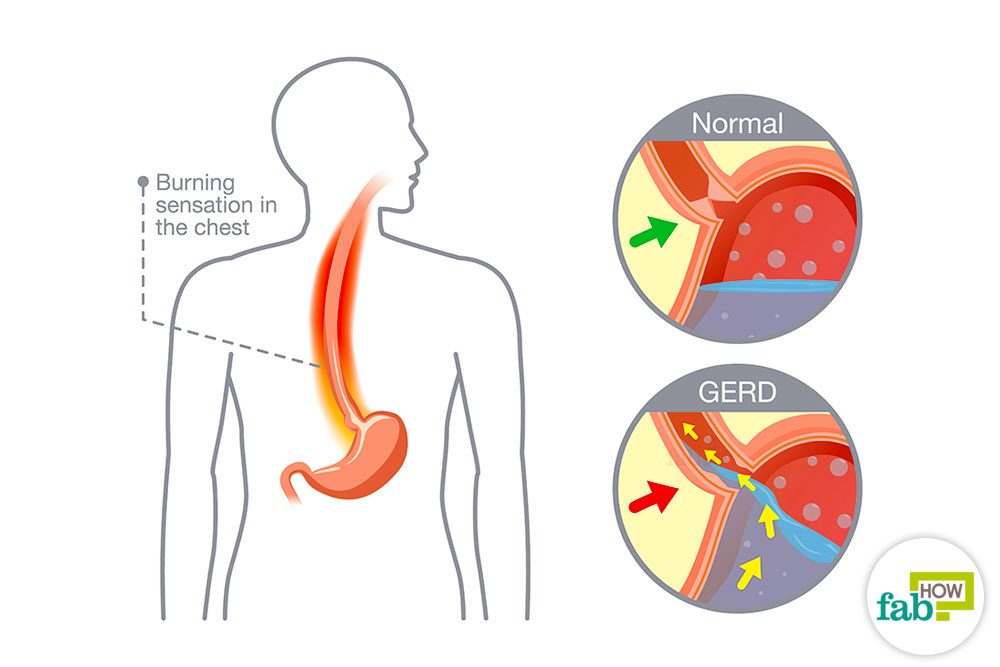
Okay I have heartburn. But what is GERD and how do I know if it is a problem? When you swallow food it should go through your esophagus (your food tube) into your stomach and stay there to be digested. A muscle called the Lower Esophageal Sphincter (LES) keeps the food and the acid used to digest it inside the stomach. Heartburn happens when your LES relaxes, even though it shouldn’t, and lets acid out into your esophagus, where it doesn’t belong. This happens to everyone from time to time. When these signs and symptoms occur at least twice each week, interfere with your daily life, or when your doctor can see damage to your esophagus (during a test), you may be diagnosed with GERD.
How do I know if I have it? GERD affects 10-20% of the US population and adults between 50 and 70 are most commonly affected. The three most common signs and symptoms are heartburn, regurgitation (food coming back up), and difficulty swallowing (dysphagia).
Along with the three most common signs there are some other symptoms that may indicate you have GERD: Pain with swallowing (odynophagia), nausea, chest pain, chronic cough, laryngitis, chronic throat clearing , voice changes / hoarseness, asthma, shortness of breath, pneumonia, bronchitis, sleep apnea, sensitive teeth, and sore throat (Pharyngitis). If your doctor thinks you may have GERD, you may be sent for an x-ray study which will look at how food moves through your esophagus and let you know for sure if reflux is taking place. Or, your doctor may start you on a medication right away to see if the symptoms go away. If they do, this can help confirm the diagnosis of GERD.
What could happen if I don’t do anything about it? Your stomach has a special protective lining that shields it from acid damage. But when this acid leaves the stomach and begins to touch structures without this special lining injury can happen. Injuries to the esophagus over time can cause conditions like esophageal stricture (narrowing of the esophagus), esophageal rings (bands of tissue that squeeze the esophagus and make it difficult for food to move through), and Barrett’s esophagus (which increases your risk of esophageal cancer). Outside the esophagus, the acid can burn your vocal cords (causing hoarseness) and your throat (making it painful or difficult for you to swallow).
What can I do to stop GERD? If you are having reflux symptoms multiple times a week you should speak to your doctor about possible tests and/or treatments. There is medication that works well to relieve GERD symptoms. In the meantime there are several lifestyle changes you can make to decrease or sometimes even eliminate the symptoms without medication. These include avoiding eating within three hours of going to bed, not lying down for at least one hour after eating, trying to sleep on your right side, increasing your water intake, avoiding overeating, losing weight, stopping smoking, avoiding spicy and acidic foods, avoiding caffeinated beverages, avoiding carbonated beverages, avoiding mint, reducing alcohol consumption, reducing stress, and chewing gum (mint flavored).
What if I am already having a voice or swallowing difficulty? North Country Hospital Rehab has skilled and experienced Speech and Swallowing therapists on staff that can provide a comprehensive evaluation of your swallowing or voice disorder. Based on this initial evaluation a treatment protocol will be established consisting of education and training in the area of your difficulty followed by the development of an exercise program individualized to help increase your skills in swallowing, voice, or both. If you are experiencing difficulties in either of these areas contact your doctor and ask whether Speech and Swallowing Services at North Country Hospital may be able to help you.
If you have further questions or would like to make an appointment, contact NCH Rehab Services, 802-334-3206.